Apixaban
 |
|
 |
|
| Clinical data | |
|---|---|
| Trade names | Eliquis |
| License data | |
| Routes of administration |
Oral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | ~50% |
| Protein binding | ~87% |
| Metabolism | CYP3A4, CYP3A5, CYP1A2 and others |
| Biological half-life | 9–14 h |
| Excretion | Biliary (75%), renal (25%) |
| Identifiers | |
|
|
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| ECHA InfoCard | 100.167.332 |
| Chemical and physical data | |
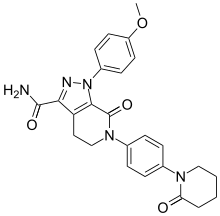
| Formula | C25H25N5O4 |
| Molar mass | 459.497 g/mol |
| 3D model (Jmol) | |
|
|
|
|
Apixaban, sold under the tradename Eliquis, is an anticoagulant for the treatment of venous thromboembolic events. It is taken by mouth. It is a direct factor Xa inhibitor.
Apixaban was approved in Europe in 2012. It was approved in the U.S. in 2014 for treatment and secondary prophylaxis of deep vein thrombosis (DVT) and pulmonary embolism (PE). It is being developed in a joint venture by Pfizer and Bristol-Myers Squibb.
Apixaban is indicated for the following:
Apixaban is recommended by the National Institute for Health and Clinical Excellence for the prevention of stroke and systemic embolism in people with non-valvular atrial fibrillation and at least one of the following risk factors: prior stroke or transient ischemic attack, age 75 years or older, diabetes mellitus, or symptomatic heart failure.
Apixaban and other newer anticoagulants (dabigatran and rivaroxaban) appear equally effective as warfarin in preventing non-hemorrhagic stroke in people with atrial fibrillation and are associated with lower risk of intracranial bleeding.
Premature discontinuation of any oral anticoagulant, including apixaban, increases thrombotic event risk. This is not due to any rebound effect from discontinuation. To reduce this risk, administering another anticoagulant is advised.
Apixaban can increase the risk of bleeding and may cause serious, potentially fatal, bleeding. Concurrent use with drugs affecting hemostasis (e.g. other anticoagulants, heparin, aspirin and other antiplatelet drugs, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, and nonsteroidal anti-inflammatory drugs (NSAIDs) can further increase the risk of bleeding.
...
Wikipedia
