Procaine
 |
|
 |
|
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| Pregnancy category |
|
| Routes of administration |
|
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | n/a |
| Metabolism | Hydrolysis by plasma esterases |
| Biological half-life | 40–84 seconds |
| Excretion | Renal |
| Identifiers | |
|
|
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| NIAID ChemDB | |
| ECHA InfoCard | 100.000.388 |
| Chemical and physical data | |
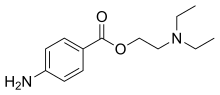
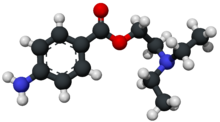
| Formula | C13H20N2O2 |
| Molar mass | 236.31 g/mol |
| 3D model (Jmol) | |
|
|
|
|
|
|
|
Procaine is a local anesthetic drug of the amino ester group. It is used primarily to reduce the pain of intramuscular injection of penicillin, and it is also used in dentistry. Owing to the ubiquity of the trade name Novocain, in some regions, procaine is referred to generically as novocaine. It acts mainly as a sodium channel blocker. Today it is used therapeutically in some countries due to its sympatholytic, anti-inflammatory, perfusion-enhancing, and mood-enhancing effects.
Procaine was first synthesized in 1905, shortly after amylocaine. It was created by the German chemist Alfred Einhorn who gave the chemical the trade name Novocaine, from the Latin nov- (meaning "new") and -caine, a common ending for alkaloids used as anesthetics. It was introduced into medical use by surgeon Heinrich Braun. Prior to the discovery of amylocaine and procaine, cocaine was the most commonly used local anesthetic. Einhorn wished his new discovery to be used for amputations, but surgeons preferred general anesthetic. Dentists, however, found it very useful.
The primary use for procaine is as an anaesthetic.
Procaine is used less frequently today since more effective (and hypoallergenic) alternatives such as lidocaine (Xylocaine) exist. Like other local anesthetics (such as mepivacaine, and prilocaine), procaine is a vasodilator, thus is often coadministered with epinephrine for the purpose of vasoconstriction. Vasoconstriction helps to reduce bleeding, increases the duration and quality of anesthesia, prevents the drug from reaching systemic circulation in large amounts, and overall reduces the amount of anesthetic required. Unlike cocaine, a vasoconstrictor, procaine does not have the euphoric and addictive qualities that put it at risk for abuse.
...
Wikipedia
