High-grade serous carcinoma
| High-grade serous carcinoma | |
|---|---|
 |
|
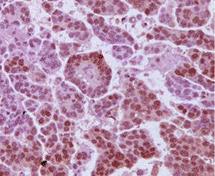
| Immunohistochemistry micrograph of androgen receptors on a HGSC tumour sample |
High-grade serous carcinoma (HGSC) is a type of tumour that arises from the serous epithelial layer in the abdominopelvic cavity and is mainly found in the ovary. HGSCs make up the majority of ovarian cancer cases and have the lowest survival rates. HGSC is distinct from low-grade serous carcinoma (LGSC) which arises from ovarian tissue, is less aggressive and is present in stage I ovarian cancer where tumours are localised to the ovary.
Although originally thought to arise from the squamous epithelial cell layer covering the ovary, HGSC is now thought to originate in the Fallopian tube epithelium. HGSC is much more invasive than LGSC with a higher fatality rate - although it is more sensitive to platinum-based chemotherapy, possibly due to its rapid growth rate. In rare cases, HGSCs can develop from LGSCs, but generally the two types arise independently of each other.
The ‘incessant ovulation’ theory is suggested by the strong correlation between the number of ovulatory cycles of an individual and their risk of ovarian cancer.
This trend is reflected in the protective effects of pregnancy, parity and breastfeeding against ovarian cancer, and similar findings in epidemiological studies that have indicated a reduction of risk associated with use of oral contraceptive pills.
Ovulation is accepted as the cause of ovarian cortical inclusion cysts, the precursor lesions of serous carcinomas, and lower numbers of these cortical inclusion cysts are thought to be the mechanism by which reducing lifetime ovulations can lower the risk of developing HGSC.
Conversely, a temporal association with menopausal hormone therapy and incidence of HGSC was found, and polycystic ovarian syndrome (PCOS) was shown to contribute to a doubling of the risk of ovarian cancer.
Endometriosis can increase risk for other ovarian cancer subtypes, but is not associated with HGSC.
More than 20% of ovarian cancer tumours have hereditary origin. The majority of these feature mutations in the tumour suppressor BRCA genes, which tend to give rise to HGSC. A mutation in BRCA1 or BRCA2 can confer a lifetime ovarian cancer risk of 40-50% and 10-20% respectively, with BRCA2 mutations strongly associated with better clinical outcomes.
...
Wikipedia
