Zolpidem
 |
|
 |
|
| Clinical data | |
|---|---|
| Trade names | originally Ambien, many names worldwide |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a693025 |
| Pregnancy category |
|
| Dependence liability |
High |
| Routes of administration |
Oral (tablet), sublingual, oromucosal (spray), rectal |
| ATC code | N05CF02 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 70% (oral) |
| Protein binding | 92% |
| Metabolism | Liver through CYP3A4 |
| Biological half-life | 2–3 hours |
| Duration of action | 3 hours |
| Excretion |
Kidney (56%) fecal (34%) |
| Identifiers | |
|
|
| CAS Number |
82626-48-0 |
| PubChem (CID) | 5732 |
| IUPHAR/BPS | 4362 |
| DrugBank |
DB00425 |
| ChemSpider |
5530 |
| UNII |
7K383OQI23 |
| KEGG |
D08690 |
| ChEBI |
CHEBI:10125 |
| ChEMBL |
CHEMBL911 |
| ECHA InfoCard | 100.115.604 |
| Chemical and physical data | |
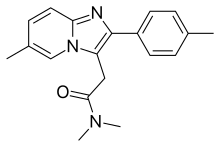
| Formula | C19H21N3O |
| Molar mass | 307.395 g/mol |
| 3D model (Jmol) | Interactive image |
|
|
|
|
|
|
|
Zolpidem (originally marketed as Ambien and available worldwide under many brand names) is a sedative primarily used for the treatment of insomnia. It works quickly, usually within 15 minutes, and has a short half-life of two to three hours. Zolpidem has not adequately demonstrated effectiveness in maintaining sleep, unless delivered in a controlled-release (CR) form. However, it is effective in initiating sleep. Its hypnotic effects are similar to those of the benzodiazepine class of drugs.
In 2013, the Food and Drug Administration required manufacturers to decrease the recommended dose for women by half, after studies showed that the medicines can leave people drowsy in the morning and at risk for motor vehicle collisions. The FDA recommended that manufacturers extend the new dosage cuts to men as well, who process the drug at a faster rate; however, the reasons men and women metabolize the drugs at different rates are still unknown. In May 2013, the FDA approved label changes specifying new dosage recommendations for zolpidem products because of concerns regarding next-morning impairment. The underlying mechanism involves GABA.
It is a short-acting nonbenzodiazepine compound of the imidazopyridine class that increases the activity of GABA, an inhibitory neurotransmitter, by binding to GABAA receptors at the same location as benzodiazepines. It is molecularly distinct from the classical benzodiazepine molecule and is classified as an imidazopyridine. Flumazenil, a benzodiazepine receptor antagonist, which is used for benzodiazepine overdose, can also reverse zolpidem's sedative/hypnotic and memory-impairing effects.
...
Wikipedia
