Susac's syndrome
| Susac's syndrome | |
|---|---|
 |
|
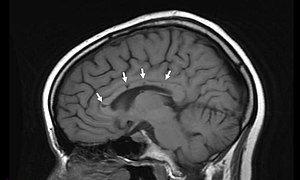
| Sagittal T1 image in a 19-year-old woman with Susac's syndrome showing the pathognomonic central callosal “holes” (microinfarcts) of SS. These residual “holes” (and sometimes, “spokes”) develop as the acute callosal changes resolve. | |
| Classification and external resources | |
| DiseasesDB | 32752 |
Susac's syndrome (Retinocochleocerebral Vasculopathy) is a microangiopathy characterized by encephalopathy, branch retinal artery occlusions and hearing loss. The cause is unknown but the current thinking is that antibodies are produced against endothelial cells in tiny arteries which leads to damage and the symptoms related to the illness. Despite this being a rare disease, there are 4 registries collecting data on the illness; two are in the United States, one is in Germany and the fourth is in Portugal.
Susac's Syndrome is named for Dr. John Susac (1940-2012), of Winter Haven, Florida, who first described it in 1979. Susac's syndrome is a very rare disease, of still unknown etiology, and many persons who experience it do not display the bizarre symptoms named here. Their speech can be affected, such as the case of a female of late teens who suffered speech issues and hearing problems, and many experience unrelenting and intense headaches and migraines, some form of hearing loss, and impaired vision. The problem usually corrects itself, but this can take up to five years. In some cases, subjects can become confused. The syndrome usually affects women around the age of 18 years, with female to male ratio of cases of 2:1.
William F. Hoyt was the first to call the syndrome "Susac Syndrome" and later Robert Daroff asked Dr. Susac to write an editorial in Neurology about the disorder and to use the eponym of Susac Syndrome in the title forever linking this disease with him.
Patients typically present with low frequency hearing loss detectable via an audiogram. Headaches are frequently present in addition to roaring tinnitus and often some degree of paranoia. Partial vision loss is often present and caused by branch retinal artery occlusions. The presence of refractile or non-refractile yellow Gass plaques in the retinal arterioles is near pathognomonic for the disease. Fluorescein angiography may demonstrate leakage in areas remote from the retinal infarctions.
Radiographic Appearance: In a recent analysis (Susac et al., 2003), MRI images from 27 patients fulfilling the diagnostic criteria of Susac's syndrome were reviewed. Multifocal supratentorial lesions were present in all patients. Most lesions were small (3 to 7 mm), though some were larger than 7 mm. All 27 patients had corpus callosum lesions. These all had a punched-out appearance on follow up MRI. Though most commonly involving white matter, many patients also had lesions in deep grey matter structures, as well as leptomeningeal enhancement. Multiple sclerosis (MS) and acute disseminated encephalomyelitis (ADEM) can mimic the MRI changes seen in patients with Susac's syndrome. However, the callosal lesions in Susac's syndrome are centrally located. In comparison, patients with MS and ADEM typically have lesions involving the undersurface of the corpus callosum. Deep gray matter involvement commonly occurs in ADEM but is very rare in MS. Leptomemingeal involvement is not typical of either MS or ADEM. What this means is that if you have 10 lesions in the brain of an MS patient, you may find one in the corpus callosum. If you have 10 lesions in a Susac patient, more than half will be in the corpus callosum.
...
Wikipedia
