Retinitis Pigmentosa
| Retinitis pigmentosa | |
|---|---|
 |
|
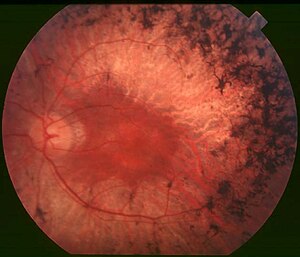
| Fundus of patient with retinitis pigmentosa, mid stage. (Bone spicule-shaped pigment deposits are present in the mid periphery along with retinal atrophy, while the macula is preserved although with a peripheral ring of depigmentation. Retinal vessels are attenuated.) | |
| Classification and external resources | |
| Specialty | Ophthalmology |
| ICD-10 | H35.5 |
| ICD-9-CM | 362.74 |
| OMIM | 268000 |
| DiseasesDB | 11429 |
| MedlinePlus | 001029 |
| Patient UK | Retinitis pigmentosa |
| MeSH | D012174 |
| GeneReviews | |
Retinitis pigmentosa (RP) is an inherited, degenerative eye disease that causes severe vision impairment due to the progressive degeneration of the rod photoreceptor cells in the retina. This form of retinal dystrophy manifests initial symptoms independent of age; thus, RP diagnosis occurs anywhere from early infancy to late adulthood. Patients in the early stages of RP first notice compromised peripheral and dim light vision due to the decline of the rod photoreceptors. The progressive rod degeneration is later followed by abnormalities in the adjacent retinal pigment epithelium (RPE) and the deterioration of cone photoreceptor cells. As peripheral vision becomes increasingly compromised, patients experience progressive "tunnel vision" and eventual blindness. Affected individuals may additionally experience defective light-dark adaptations, nyctalopia (night blindness), and the accumulation of bone spicules in the fundus.
The initial retinal degenerative symptoms of Retinitis Pigmentosa are characterized by decreased night vision (nyctalopia) and the loss of the mid-peripheral visual field. The rod photoreceptor cells, which are responsible for low-light vision and are orientated in the retinal periphery, are the retinal processes affected first during non-syndromic forms of this disease. Visual decline progresses relatively quickly to the far peripheral field, eventually extending into the central visual field as tunnel vision increases. Visual acuity and color vision can become compromised due to accompanying abnormalities in the cone photoreceptor cells, which are responsible for color vision, visual acuity, and sight in the central visual field. The progression of disease symptoms occurs in a symmetrical manner, with both the left and right eyes experiencing symptoms at a similar rate.
A variety of indirect symptoms characterize Retinitis Pigmentosa along with the direct effects of the initial rod photoreceptor degeneration and later cone photoreceptor decline. Phenomena such as photophobia, which describes the event in which light is perceived as an intense glare, and photopsia, the presence of blinking or shimmering lights within the visual field, often manifest during the later stages of RP. Findings related to RP have often been characterized in the fundus of the eye as the Ophthalamic triad. This includes the development of a mottled appearance of the retinal pigment epithelium (RPE) caused by bone spicule formation, a waxy appearance of the optic nerve, and the attentuation of blood vessels in the retina.
...
Wikipedia
