MDR-TB
| Multi-drug-resistance tuberculosis | |
|---|---|
 |
|
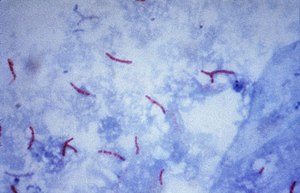
| Mycobacterium tuberculosis bacteria seen by microscope | |
| Classification and external resources | |
| ICD-10 | Z16.24 |
| MeSH | D018088 |
Multi-drug-resistant tuberculosis (MDR-TB) is a form of tuberculosis (TB) infection caused by bacteria that are resistant to treatment with at least two of the most powerful first-line anti-TB medications (drugs), isoniazid and rifampin. Some forms of TB are also resistant to second-line medications, and are called extensively drug-resistant TB (XDR-TB).
Tuberculosis is caused by infection with the bacteria Mycobacterium tuberculosis. Almost one in four people in the world are infected with TB bacteria. Only when the bacteria become active do people become ill with TB. Bacteria become active as a result of anything that can reduce the person’s immunity, such as HIV, advancing age, diabetes or other immunocompromising illnesses. TB can usually be treated with a course of four standard, or first-line, anti-TB drugs (i.e., isoniazid, rifampin and any fluoroquinolone).
However, beginning with the first antibiotic treatment for TB in 1943, some strains of the TB bacteria developed resistance to the standard drugs through genetic changes (see mechanisms.) This process accelerates if incorrect or inadequate treatments are used, leading to the development and spread of multidrug-resistant TB (MDR-TB). Incorrect or inadequate treatment may be due to use of the wrong medications, use of only one medication (standard treatment is at least two drugs), not taking medication consistently or for the full treatment period (treatment is required for several months). Treatment of MDR-TB requires second-line drugs (i.e., fluoroquinolones, aminoglycosides, and others), which in general are less effective, more toxic and much more expensive than first-line drugs. If these second-line drugs are prescribed or taken incorrectly, further resistance can develop leading to XDR-TB.
...
Wikipedia
