Aclidinium bromide
 |
|
| Clinical data | |
|---|---|
| Trade names | Bretaris Genuair, Eklira Genuair, Tudorza Pressair |
| AHFS/Drugs.com | tudorza |
| License data |
|
| Pregnancy category |
|
| Routes of administration |
Inhalation |
| ATC code | R03BB05 (WHO) |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | <5% (in system) 30% (in lung) |
| Metabolism | Ester hydrolysis |
| Biological half-life | 2–3 hrs |
| Duration of action | >24 hrs |
| Excretion | 65% urine, 33% faeces |
| Identifiers | |
|
|
| CAS Number |
320345-99-1 |
| PubChem (CID) | 11519741 |
| DrugBank |
DB08897 |
| ChemSpider |
9694529 |
| UNII |
UQW7UF9N91 |
| KEGG |
D08837 |
| ChEBI |
CHEBI:65344 |
| ChEMBL |
CHEMBL551466 |
| Chemical and physical data | |
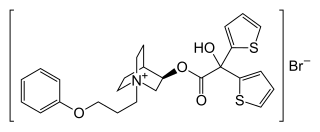
| Formula | C26H30BrNO4S2 |
| Molar mass | 564.55 g·mol−1 |
| 3D model (Jmol) | Interactive image |
|
|
|
|
|
|
|
Aclidinium bromide (INN) is a long-acting, inhaled muscarinic antagonist (LAMA) approved in the US on July 24, 2012 as a maintenance treatment for chronic obstructive pulmonary disease (COPD).
Evidence shows that it can improve quality of life and prevent hospitalization in those with COPD. However, it does not appear to affect the risk of death or the frequency steroids are needed. It is unclear if it differs from the similar medication tiotropium or other commonly used medications from the class of LAMAs.
Aclidinium is delivered via a multidose dry powder inhaler, the Genuair inhaler.
The substance is generally well tolerated. Common side effects (in more than 1% of patients) are sinusitis, nasopharyngitis, headache, cough, diarrhoea and nausea. The latter is less common under the drug than under placebo. Skin reactions such as rash, as well as side effects that are typical of muscarinic antagonists (fast heart rate, palpitations, and urinary retention), occur in less than 1% of patients.
A small increase of cardiovascular risk cannot be excluded from available data. Patients with relevant cardiovascular diseases were excluded from studies.
No systematic interaction studies have been performed. It is expected that adverse effects of aclidinium increase if it is combined with other muscarinic antagonists. In clinical practice, no interactions with other COPD medications such as glucocorticoids, β2-adrenergic agonists and theophylline have been described. As aclidinium does not relevantly interact with liver enzymes or P-glycoprotein, and is quickly metabolized as soon as it reaches the bloodstream, it is considered to have a very low potential for interactions.
...
Wikipedia
