Yersinia pseudotuberculosis
| Yersinia pseudotuberculosis | |
|---|---|
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Proteobacteria |
| Class: | Gammaproteobacteria |
| Order: | Enterobacteriales |
| Family: | Enterobacteriaceae |
| Genus: | Yersinia |
| Species: | Y. pseudotuberculosis |
| Binomial name | |
|
Yersinia pseudotuberculosis (Pfeiffer 1889) Smith & Thal 1965 |
|
| Yersinia pseudotuberculosis | |
|---|---|
 |
|
| Yersinia scanned with electron micrograph | |
| Classification and external resources | |
| Specialty | infectious disease |
| ICD-10 | A04.8, A28.2 |
| DiseasesDB | 14237 |
| eMedicine | article/226871 |
| MeSH | D015012 |
| YpM | |||||||||
|---|---|---|---|---|---|---|---|---|---|
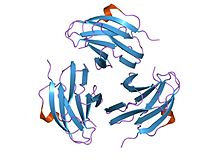
crystal structure of yersinia pseudotuberculosis-derived mitogen (ypm)
|
|||||||||
| Identifiers | |||||||||
| Symbol | YpM | ||||||||
| Pfam | PF09144 | ||||||||
| InterPro | IPR015227 | ||||||||
| SCOP | 1pm4 | ||||||||
| SUPERFAMILY | 1pm4 | ||||||||
|
|||||||||
| Available protein structures: | |
|---|---|
| Pfam | structures |
| PDB | RCSB PDB; PDBe; PDBj |
| PDBsum | structure summary |
Yersinia pseudotuberculosis is a Gram-negative bacterium that causes Far East scarlet-like fever in humans, who occasionally get infected zoonotically, most often through the food-borne route. Animals are also infected by Y. pseudotuberculosis. The bacterium is urease positive.
In animals, Y. pseudotuberculosis can cause tuberculosis-like symptoms, including localized tissue necrosis and granulomas in the spleen, liver, and lymph nodes.
In humans, symptoms of Far East scarlet-like fever are similar to those of infection with Yersinia enterocolitica (fever and right-sided abdominal pain), except that the diarrheal component is often absent, which sometimes makes the resulting condition difficult to diagnose. Y. pseudotuberculosis infections can mimic appendicitis, especially in children and younger adults, and, in rare cases, the disease may cause skin complaints (erythema nodosum), joint stiffness and pain (reactive arthritis), or spread of bacteria to the blood (bacteremia).
Far East scarlet-like fever usually becomes apparent five to 10 days after exposure and typically lasts one to three weeks without treatment. In complex cases or those involving immunocompromised patients, antibiotics may be necessary for resolution; ampicillin, aminoglycosides, tetracycline, chloramphenicol, or a cephalosporin may all be effective.
...
Wikipedia
