Ventricular fibrillation
| Ventricular fibrillation | |
|---|---|
 |
|
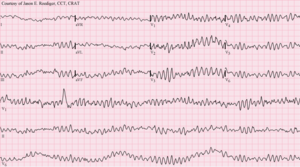
| 12-lead ECG showing ventricular fibrillation | |
| Classification and external resources | |
| Specialty | Cardiology |
| ICD-10 | I49.0 |
| ICD-9-CM | 427.41 |
| DiseasesDB | 13798 |
| MedlinePlus | 007200 |
| Patient UK | Ventricular fibrillation |
| MeSH | D014693 |
Ventricular fibrillation (V-fib or VF) is when the heart quivers instead of pumping due to disorganized electrical activity in the ventricles. It results in cardiac arrest with loss of consciousness and no pulse. This is followed by irreversible death in the absence of treatment. Ventricular fibrillation is found initially in about 10% of people in cardiac arrest.
Ventricular fibrillation can occur due to coronary heart disease, valvular heart disease, cardiomyopathy, Brugada syndrome, long QT syndrome, or intracranial hemorrhage. Diagnosis is by an electrocardiogram (ECG) showing irregular unformed QRS complexes without any clear P waves. An important differential diagnosis is torsades de pointes.
Treatment is with cardiopulmonary resuscitation (CPR) and defibrillation. Biphasic defibrillation may be better than monophasic. The medication epinephrine or amiodarone may be given if initial treatments are not effective. Rates of survival are about 46%.
Ventricular fibrillation is a cause of cardiac arrest and sudden cardiac death. The ventricular muscle twitches randomly rather than contracting in a co-ordinated fashion (from the apex of the heart to the outflow of the ventricles), and so the ventricles fail to pump blood around the body - because of this, it is classified as a cardiac arrest rhythm, and patients in V-fib should be treated with cardiopulmonary resuscitation and prompt defibrillation. Left untreated, ventricular fibrillation is rapidly fatal as the vital organs of the body, including the heart, are starved of oxygen, and as a result patients in this rhythm will not be conscious or responsive to stimuli. Prior to cardiac arrest, patients may complain of varying symptoms depending on the underlying cause. Patients may exhibit signs of agonal breathing, which to the layperson can look like normal spontaneous breathing, but it is in fact a sign of hypoperfusion of the brainstem.
...
Wikipedia
