Sixth nerve palsy
| Sixth nerve palsy | |
|---|---|
| Synonyms | lateral rectus palsy, VIth cranial nerve palsy, abducens nerve palsy |
 |
|
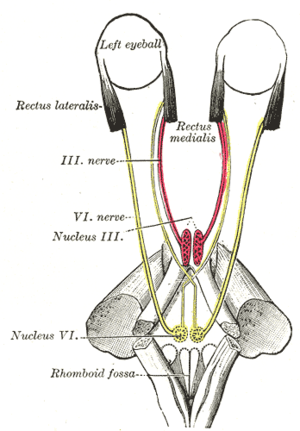
| Figure showing the mode of innervation of the Recti medialis and lateralis of the eye. | |
| Classification and external resources | |
| Specialty | ophthalmology |
| ICD-10 | H49.2 |
| ICD-9-CM | 378.54 |
| DiseasesDB | 2868 |
| eMedicine | oph/158 |
| MeSH | C10.292.150 |
Sixth nerve palsy, or abducens nerve palsy, is a disorder associated with dysfunction of cranial nerve VI (the abducens nerve), which is responsible for causing contraction of the lateral rectus muscle to abduct (i.e., turn out) the eye. The inability of an eye to turn outward results in a convergent strabismus or esotropia of which the primary symptom is diplopia (commonly known as double vision) in which the two images appear side-by-side. The condition is commonly unilateral but can also occur bilaterally.
The unilateral abducens nerve palsy is the most common of the isolated ocular motor nerve palsies.
The nerve dysfunction induces esotropia, a convergent squint on distance fixation. On near fixation the affected individual may have only a latent deviation and be able to maintain binocularity or have an esotropia of a smaller size. Patients sometimes adopt a face turn towards the side of the affected eye, moving the eye away from the field of action of the affected lateral rectus muscle, with the aim of controlling diplopia and maintaining binocular vision.
Diplopia is typically experienced by adults with VI nerve palsies, but children with the condition may not experience diplopia due to suppression. The neuroplasticity present in childhood allows the child to 'switch off' the information coming from one eye, thus relieving any diplopic symptoms. Whilst this is a positive adaptation in the short term, in the long term it can lead to a lack of appropriate development of the visual cortex giving rise to permanent visual loss in the suppressed eye; a condition known as amblyopia.
Because the nerve emerges near the bottom of the brain, it is often the first nerve compressed when there is any rise in intracranial pressure. Different presentations of the condition, or associations with other conditions, can help to localize the site of the lesion along the VIth cranial nerve pathway.
...
Wikipedia
