Pseudomyxoma peritonei
| Pseudomyxoma Peritonei | |
|---|---|
 |
|
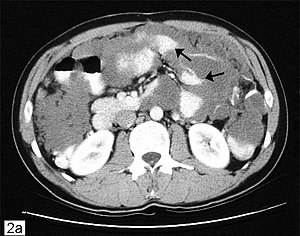
| Computed tomographic scan of an abdomen showing pseudomyxoma peritonei with multiple peritoneal masses (arrow) with "scalloping effect" seen. | |
| Classification and external resources | |
| Specialty | oncology |
| ICD-10 | C78.6 |
| ICD-9-CM | 197.6 |
| ICD-O | M8480 |
| DiseasesDB | 31498 |
| eMedicine | med/1795 |
| MeSH | D011553 |
| Orphanet | 26790 |
Pseudomyxoma peritonei (PMP) is a clinical condition caused by cancerous cells (mucinous adenocarcinoma) that produce abundant mucin or gelatinous ascites. The tumors cause fibrosis of tissues and impede digestion or organ function, and if left untreated, the tumors and mucin they produce will fill the abdominal cavity. This will result in compression of organs and will destroy the function of colon, small intestine, stomach, or other organs. Prognosis with treatment in many cases is optimistic, but the disease is lethal if untreated, with death by cachexia, bowel obstruction, or other types of complications.
This disease is most commonly caused by an appendiceal primary cancer (cancer of the appendix); mucinous tumors of the ovary have also been implicated, although in most cases ovarian involvement is favored to be a metastasis from an appendiceal or other gastrointestinal source. Disease is typically classified as low- or high-grade (with signet ring cells). When disease presents with low-grade histologic features the cancer rarely spreads through the lymphatic system or through the bloodstream.
There is substantial debate regarding histopathologic classification of pseudomyxoma peritonei. In 1995, Ronnett et al. proposed separating pseudomyxoma peritonei cases into two diagnostic categories: adenoma (disseminated peritoneal adenomucinosis, DPAM) or carcinoma (peritoneal mucinous carcinomatosis, PMCA) with a third category reserved for cases with intermediate features. In this classification system, cases of DPAM were characterized by peritoneal lesions composed of abundant extracellular mucin containing scant simple to focally proliferative mucinous epithelium with little cytologic atypia or mitotic activity (in other words, most cells looked fairly normal and there was no evidence of mitosis which would indicate that cells were rapidly dividing), with or without an associated appendiceal mucinous adenoma. Cases of PMCA were characterized by peritoneal lesions composed of more abundant mucinous epithelium with the architectural and cytologic features of carcinoma (irregular cells, evidence that cells were rapidly dividing, and other criteria), with or without an associated primary mucinous adenocarcinoma. Bradley et al. (2007) argued that continued use of non-malignant terms, i.e., adenoma, for those frequent cases with low-grade features (such as DPAM), is misleading because pseudomyxoma peritonei is a disease state that results from invasion of the abdominal cavity by cells with uncontrolled growth. Bradley states that an adenoma, by definition, is a tumor confined to the appendiceal mucosa with absolutely no evidence of invasion beyond the muscularis mucosae.
...
Wikipedia
