Pseudoaneurysm
| Pseudoaneurysm | |
|---|---|
 |
|
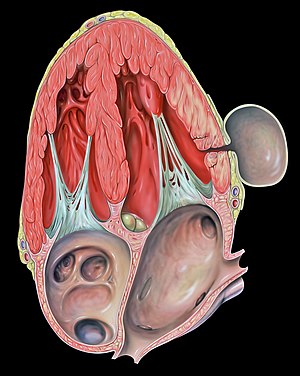
| Pseudoaneurysm of the left ventricle, four-chamber echocardiography view | |
| Classification and external resources | |
| Specialty | angiology, cardiology |
| MeSH | D017541 |
A pseudoaneurysm, also known as a false aneurysm, is a collection of blood that forms between the two outer layers of an artery, the muscularis and the adventitia. It is usually caused by a penetrating injury to the vessel, which then bleeds, but forms a space between the above two layers, rather than exiting the vessel. It may be pulsatile, and can resemble a true aneurysm. A true aneurysm involves all three layers of the blood vessel. A dissecting aneurysm is when blood from the vessel lumen tracks between the two inner layers, the intima and the muscularis. This can cause blockage of the flow. A perivascular hematoma is a collection of blood that is external to the three vessel layers. Due to being close to the vessel, it can also be pulsatile, and can be mistaken for a pseudoaneyryam or aneurysm.
Femoral pseudoaneurysms may complicate up to 8% of vascular interventional procedures. Small pseudoaneurysms can spontaneously clot, while others need definitive treatment.
A pseudoaneurysm may also occur in a chamber of the heart following myocardial damage due to ischemia or trauma. A pseudoaneurysm of the left ventricle is a potentially lethal complication from a myocardial infarction.
Pseudoaneurysms usually present as a painful, tender, pulsatile mass. The overlying skin is sometimes erythematous (red). They can sometimes be confused with abscesses. The patient may describe a history of catheterization or trauma, and they may note that the pulsatile mass is gradually expanding.
The diagnosis should be suspected if the patient has a history of arterial trauma. This can include arterial access for catheterization (i.e. the common femoral artery), blunt trauma (i.e. to an extremity), or penetrating trauma (i.e. gunshot or blast injury). Blunt or penetrating trauma can cause a disruption in the arterial wall, leading to a pseudoaneurysm. A patient with such a history who presents with a painful, pulsatile, tender mass at the site of catheterization or trauma should be suspected to have a pseudoaneurysm. The diagnosis should be confirmed using Duplex ultrasonography, which will reveal arterial blood flow into the pseudoaneurysm. A CT angiogram or conventional angiogram can also diagnose a pseudoaneurysm.
...
Wikipedia
