Organ rejection
| Transplant rejection | |
|---|---|
 |
|
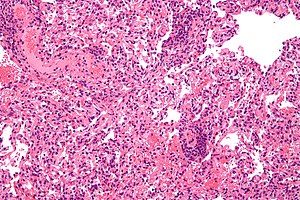
| Micrograph showing lung transplant rejection. Lung biopsy. H&E stain. | |
| Classification and external resources | |
| Specialty | emergency medicine |
| ICD-10 | T86 |
| MedlinePlus | 000815 |
| MeSH | D006084 |
Transplant rejection occurs when transplanted tissue is rejected by the recipient's immune system, which destroys the transplanted tissue. Transplant rejection can be lessened by determining the molecular similitude between donor and recipient and by use of immunosuppressant drugs after transplant.
The first successful organ transplant, performed in 1954 by Joseph Murray, involved identical twins, and so no rejection was observed. Otherwise, the number of mismatched gene variants, namely alleles, encoding cell surface molecules called (MHC), classes I and II, correlate with the rapidity and severity of transplant rejection. In humans MHC is also called human leukocyte antigen (HLA).
Though cytotoxic-crossmatch assay can predict rejection mediated by cellular immunity, genetic-expression tests specific to the organ type to be transplanted, for instance AlloMap Molecular Expression Testing, have a high negative predictive value. Transplanting only ABO-compatible grafts (matching blood groups between donor and recipient) helps prevent rejection mediated by humoral immunity.
Because very young children (generally under 12 months, but often as old as 24 months) do not have a well-developed immune system, it is possible for them to receive organs from otherwise incompatible donors. This is known as ABO-incompatible (ABOi) transplantation. Graft survival and patient mortality is approximately the same between ABOi and ABO-compatible (ABOc) recipients. While focus has been on infant heart transplants, the principles generally apply to other forms of solid organ transplantation.
The most important factors are that the recipient have not produced isohemagglutinins, and that they have low levels of T cell-independent antigens. UNOS regulations allow for ABOi transplantation in children under two years of age if isohemagglutinin titers are 1:4 or below, and if there is no matching ABOc recipient. Studies have shown that the period under which a recipient may undergo ABOi transplantation may be prolonged by exposure to nonself A and B antigens. Furthermore, should the recipient (for example, type B-positive with a type AB-positive graft) require eventual retransplantation, the recipient may receive a new organ of either blood type.
...
Wikipedia
