Mediastinal mass
| Mediastinal tumor | |
|---|---|
 |
|
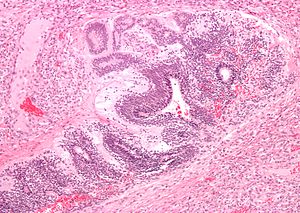
| Micrograph of the primitive neuroepithelium of an immature teratoma of the mediastinum. H&E stain. | |
| Classification and external resources | |
| Specialty | oncology |
| ICD-10 | C38.1-C38.3 |
| ICD-9-CM | 786.6-164.9 |
| MedlinePlus | 001086 |
| MeSH | D008479 |
The mediastinum is the cavity that separates the lungs from the rest of the chest. It contains the heart, esophagus, trachea, thymus, and aorta. The mediastinum has three main parts: the anterior mediastinum (front), the middle mediastinum, and the posterior mediastinum (back).
The most common mediastinal masses are neurogenic tumors (20% of mediastinal tumors), usually found in the posterior mediastinum, followed by thymoma (15-20%) located in the anterior mediastinum.
Masses in the anterior portion of the mediastinum can include thymoma, lymphoma, pheochromocytoma, germ cell tumors including teratoma, thyroid tissue, and parathyroid lesions. Masses in this area are more likely to be malignant than those in other compartments.
Masses in the posterior portion of the mediastinum tend to be neurogenic in origin, and in adults tend to be of neural sheath origin including neurilemomas and neurofibromas.
Lung cancer typically spreads to the lymph nodes in the mediastinum.
In several editions of Physical Diagnosis, concerning mediastinal tumors the author writes:
Many signs and symptoms of a mediastinal tumor do not distinguish between these two principal classes of mediastinal tumor. However, on a radiograph usually the former class will have an irregular shape and the latter class will have a smooth spherical or ovoid shape. A large minority of patients with a mediastinal teratoma (including dermoid cyst) will cough up hair. For a differential diagnosis, the key is to exclude aneurism.
Most common primary anterior mediastinal tumor (20%) in adults but rarely seen in children. It can be classified as lymphocytic, epithelial, or spindle cell histologies, but the clinical significance of these classifications is controversial. Tonofibrils seen under electron microscopy can differentiate thymoma from other tumors such as carcinoid, Hodgkin's, and seminoma. Patients are usually asymptomatic but can present with myasthenia gravis-related symptoms, substernal pain, dyspnea, or cough. Invasive tumors can produce compression effects such as superior vena cava syndrome. (3,4) Thymomas are diagnosed with CT or MRI revealing a mass in anterior mediastinum. Therapy in stage I tumors consists of surgical resection with good prognosis. Stage II-III requires maximal resection possible followed by radiation. Stage IV disease requires addition of cisplatin-based chemotherapy in addition to those in stage II and III. For those with invasive thymoma, treatment is based on induction chemotherapy, surgical resection, and post-surgical radiation. 5-year survival for invasive thymoma is between 12-54% regardless of any myasthenia gravis symptoms (5,6).
...
Wikipedia
