Lymphangioleiomyomatosis
| Lymphangioleiomyomatosis | |
|---|---|
 |
|
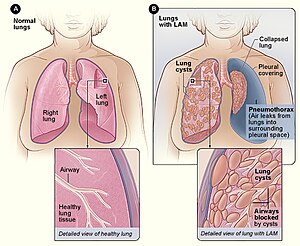
| Figure A shows the location of the lungs and airways in the body. The inset image shows a cross-section of a healthy lung. Figure B shows a view of the lungs with LAM and a collapsed lung (pneumothorax). The inset image shows a cross-section of a lung with LAM. | |
| Classification and external resources | |
| ICD-10 | J84.81 |
| ICD-9-CM | 516.4 |
| ICD-O | 9174/1 |
| OMIM | 606690 |
| DiseasesDB | 30755 |
| eMedicine | med/1348 radio/415 |
| MeSH | D018192 |
Lymphangioleiomyomatosis (LAM) is a rare, progressive and systemic disease that typically results in cystic lung destruction. It predominantly affects women, especially during childbearing years.
The average age of onset is the early to mid 30s. Exertional dyspnea and spontaneous pneumothorax have been reported as the initial presentation of the disease in 49% and 46% of patients, respectively.
Diagnosis is typically delayed 5 to 6 years. The condition is often misdiagnosed as asthma or chronic obstructive pulmonary disease. The first pneumothorax precedes the diagnosis of LAM in 82% of patients. The consensus clinical definition of LAM includes multiple symptoms:
Lung destruction in LAM is a consequence of diffuse infiltration by neoplastic smooth muscle-like cells that invade all lung structures including the lymphatics, airway walls, blood vessels and interstitial spaces. The consequences of vessel and airway obstruction include chylous fluid accumulations, hemoptysis, airflow obstruction and pneumothorax. The typical disease course displays progressive dyspnea on exertion, spaced by recurrent pneumothoraces and in some patients, chylous pleural effusions or ascites.
Most people have dyspnea on exertion with daily activities by 10 years after symptom onset. Many patients require supplemental oxygen over that interval.
LAM occurs in two settings: in the disease tuberous sclerosis complex (TSC-LAM) and in a sporadic form, in women who do not have TSC (sporadic LAM). In both settings, genetic evidence indicates that LAM is caused by inactivating or “loss of function” mutations in the TSC1 or TSC2 genes, which were cloned in 1997 and 1993 respectively. The TSC1 gene is located on chromosome 9q34 and the TSC2 gene is located on chromosome 16p13. TSC-LAM occurs in women who have germline mutations in either the TSC1 or the TSC2 gene.
Sporadic LAM is primarily associated with somatic TSC2 gene mutations. Germline and somatic mutations in LAM include many types of mutations spread across the genes, with no clear “hot spots,” including missense changes, in-frame deletions and nonsense mutations. Because of the large size of the genes (together they have more than 60 exons) and because mutations can be located virtually anywhere within the genes, mutation detection is often challenging.
...
Wikipedia
