Hay Fever
| Allergic rhinitis | |
|---|---|
| Synonyms | hay fever, pollinosis |
 |
|
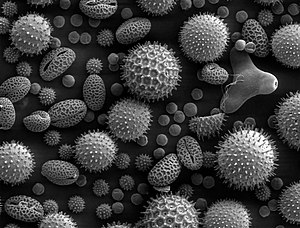
| Pollen grains from a variety of plants. Enlarged 500 times and about 0.4 mm wide. | |
| Classification and external resources | |
| Specialty | Allergy and immunology |
| ICD-10 | J30 |
| ICD-9-CM | 477 |
| OMIM | 607154 |
| DiseasesDB | 31140 |
| MedlinePlus | 000813 |
| eMedicine | ent/194 med/104, ped/2560 |
| Patient UK | Allergic rhinitis |
| MeSH | D012221 |
Allergic rhinitis, also known as hay fever, is a type of inflammation in the nose which occurs when the immune system overreacts to allergens in the air. Signs and symptoms include a runny or stuffy nose, sneezing, red, itchy, and watery eyes, and swelling around the eyes. The fluid from the nose is usually clear. Symptom onset is often within minutes following exposure and they can affect sleep, the ability to work, and the ability to concentrate at school. Those whose symptoms are due to pollen typically develop symptoms during specific times of the year. Many people with allergic rhinitis also have asthma, allergic conjunctivitis, or atopic dermatitis.
Allergic rhinitis is typically triggered by environmental allergens such as pollen, pet hair, dust, or mold. Inherited genetics and environmental exposures contribute to the development of allergies. Growing up on a farm and having multiple siblings decreases the risk. The underlying mechanism involves IgE antibodies attaching to the allergen and causing the release of inflammatory chemicals such as histamine from mast cells. Diagnosis is usually based on a medical history in combination with a skin prick test or blood tests for allergen-specific IgE antibodies. These tests, however, are sometimes falsely positive. The symptoms of allergies resemble those of the common cold; however, they often last for more than two weeks and typically do not include a fever.
Exposure to animals in early life might reduce the risk of developing allergies to them later. A number of medications may improve symptoms including nasal steroids, antihistamines such as diphenhydramine, cromolyn sodium, and leukotriene receptor antagonists such as montelukast. Medications are, however, not sufficient or are associated with side effects in many people. Exposing people to larger and larger amounts of allergen, known as allergen immunotherapy is often effective. The allergen may be given as injections just under the skin or as a tablet under the tongue. Treatment typically lasts three to five years after which benefits may be prolonged.
...
Wikipedia
