Fingolimod
 |
|
 |
|
| Clinical data | |
|---|---|
| Trade names | Gilenya |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category |
|
| Routes of administration |
By mouth (capsules) |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
|
|
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
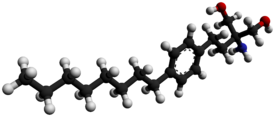
| Formula | C19H33NO2 |
| Molar mass | 307.471 g/mol |
| 3D model (Jmol) | |
|
|
|
|
|
|
|
Fingolimod (INN, trade name Gilenya, Novartis) is an immunomodulating drug, mostly used for treating multiple sclerosis (MS). It has reduced the rate of relapses in relapsing-remitting multiple sclerosis by approximately one-half over a two-year period. Fingolimod is a sphingosine-1-phosphate receptor modulator, which sequesters lymphocytes in lymph nodes, preventing them from contributing to an autoimmune reaction.
Fingolimod is used in the treatment of the relapsing form of multiple sclerosis. Its effect in those with primary progressive MS is not clear. May also be used in chronic inflammatory demyelinating polyneuropathy. It was originally proposed as an antirejection medication indicated after transplantation but it failed to show any significant benefit in post-transplantation clinical trials.
The most common side effects of fingolimod have been head colds, headache, and fatigue. A few cases of skin cancer have been reported, which has also been reported in patients taking natalizumab (Tysabri), an approved MS drug. Fingolimod has also been associated with potentially fatal infections, bradycardia and, recently, a case of hemorrhaging focal encephalitis, an inflammation of the brain with bleeding. Two people died: one due to brain herpes infection, and a second one due to zoster. It is unclear whether the drug was responsible for the events. At least three cases of progressive multifocal leukoencephalopathy had also occurred as of 2015.
Fingolimod has also been known to cause macular edema, resulting in decreased vision.
The European Medicines Agency has advised doctors to increase their level of monitoring of people after the first dose of the medicine. This includes electrocardiogram (ECG) monitoring before treatment and then continuously for the first six hours after the first dose, and measurement of blood pressure and heart rate every hour.
...
Wikipedia
