Dexlansoprazole
 |
|
| Clinical data | |
|---|---|
| Trade names | Kapidex, Dexilant |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a695020 |
| License data |
|
| Pregnancy category |
|
| Routes of administration |
by mouth |
| Drug class | proton pump inhibitor |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Excretion | 50% renal and 47% in the feces |
| Identifiers | |
|
|
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| Chemical and physical data | |
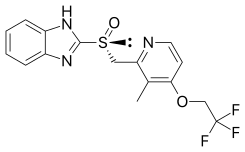
| Formula | C16H14F3N3O2S |
| Molar mass | 369.363 g/mol |
| 3D model (Jmol) | |
|
|
|
|
|
|
|
Dexlansoprazole (trade names Kapidex, Dexilant) is a proton pump inhibitor (PPI) that is marketed by Takeda Pharmaceuticals for the treatment of erosive esophagitis and gastro-oesophageal reflux disease. It is similar in effectiveness to other PPIs.
Dexlansoprazole is used to heal and maintain healing of erosive esophagitis and to treat heartburn associated with gastroesophageal reflux disease (GERD). It lasts longer than lansoprazole, to which it is chemically related, and needs to be taken less often. There is not good evidence that it works better than other PPIs.
The most significant adverse reactions (≥2%) reported in clinical trials were diarrhea, abdominal pain, nausea, upper respiratory tract infection, vomiting, and flatulence.
Like lansoprazole, dexlansoprazole permanently binds to the proton pump and blocks it, preventing the formation of gastric acid.
Dexlansoprazole is the (R)-(+)-enantiomer of lansoprazole, which is a racemic mixture of its (R)-(+) and (S)-(−)-enantiomers. The Takeda drug has a dual release pharmaceutical formulation, with two types of granules of dexlansoprazole, each with a coating that dissolves at a different pH level.
Dexlansoprazole ((R)-(+)-lansoprazole) has the same binding affinity to the proton pump as the (S)-enantiomer, but is associated with a three- to five-fold greater area under the plasma drug concentration time curve (AUC) compared with (S)-lansoprazole. With its dual release pharmaceutical formulation, the first quick release produces a plasma peak concentration about one hour after application, with a second retarded release producing another peak about four hours later. As of November 2009[update], clinical relevance of this form of release has yet to be shown.
...
Wikipedia
