Acanthamoeba
| Acanthamoeba | |
|---|---|
 |
|
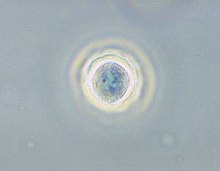
| Phase contrast micrograph of an Acanthamoeba polyphaga cyst. | |
| Scientific classification | |
| Domain: | Eukaryota |
| (unranked): | Amoebozoa |
| (unranked): | Discosea |
| Order: | Centramoebida |
| Family: | Acanthamoebidae |
| Genus: | Acanthamoeba |
Acanthamoeba is a genus of amoebae, one of the most common single-celled eukaryote in soil, and frequently found in fresh water and other habitats. Acanthamoeba has two evolutive forms, the metabolically active trophozoite and a dormant, stress resistant cyst. Trophozoites are small, usually 15 to 35 μm in length and amoeboid in shape. In nature, Acanthamoeba species are free-living bacterivores, but in certain situations they can cause infections (Acanthamebiasis) in humans and other animals.
Acanthamoeba spp. are among the most prevalent protozoa found in the environment. They are distributed worldwide, and have been isolated from soil, air, sewage, seawater, chlorinated swimming pools, domestic tap water, bottled water, dental treatment units, hospitals, air-conditioning units, and contact lens cases. Additionally, Acanthamoeba have been isolated from human skin, nasal cavities, throats, and intestines, as well as plants and other mammals.
Diseases caused by Acanthamoeba include keratitis and granulomatous amoebic encephalitis (GAE). The latter is often but not always seen in immunosuppressed patients. GAE is caused by the amoeba entering the body through an open wound then spreading to the brain. The combination of host immune response and amoebal proteases causes massive brain swelling resulting in death in ~95% of those infected.
Granulomatous amoebic encephalitis is caused by amoeba infection of the central nervous system. It is characterized by neurological symptoms including headache, seizures, and mental status abnormalities. These worsen progressively over weeks to months, leading to death in most patients. Infection is generally associated with underlying conditions such as immunodeficiency, diabetes, malignancies, malnutrition, systemic lupus erythematosus, and alcoholism. The parasite enters the body through cuts in the skin or by being inhaled into the upper respiratory tract. The parasite then spreads through the blood into the central nervous system. Acanthamoeba crosses the blood–brain barrier by means that are not yet understood. Subsequent invasion of the connective tissue and induction of pro-inflammatory responses leads to neuronal damage that can be fatal within days. Pure granulomatous lesions are rare in patients with AIDS and other related immunodeficiency states as the patients do not have adequate numbers of CD+ve T-cells to mount a granulomatous response to Acanthamoeba infection in CNS and other organ and tissues. A perivascular cuffing with amoebae in necrotic tissue is usual finding in the AIDS and related T-cell immunodeficiency conditions. A post mortem biopsy reveals severe oedema and hemorrhagic necrosis. A patient who has contracted this illness usually displays subacute symptoms, including altered mental status, headaches, fever, neck stiffness, seizures, focal neurological signs (such as cranial nerve palsies and coma), all leading to death within one week to several months. Due to the rarity of this parasite and a lack of knowledge, there are currently no good diagnoses or treatments for Acanthamoeba infection. Acanthamoeba keratitis cases in the past, when were managed by atropine given as an adjuvant therapy without anti-parasitic drugs added to the regime, had been reported to halt the vision loss. Recent publications debate these successes related to an action of Atropine on muscarinic receptors on Acanthamoeba spp.
...
Wikipedia
